

| Drug Name: | Lorazepam (Ativan Generic) |
|---|---|
| Tablet Strength: | 2 mg |
| Best Price: | $164.95 (Per Pill $2.75) |
| Where to buy | OnlinePharmacy |
Lorazepam is a short- to intermediate-acting benzodiazepine widely used for the management of acute anxiety, seizure activity, and muscle-related tension impacting speech and swallowing. Its pharmacological properties make it highly effective in urgent care situations and in multidisciplinary rehabilitation protocols where immediate reduction of central excitability is required. Lorazepam acts as a central nervous system depressant, delivering prompt relief in episodes of panic, convulsions, or motor instability, with particular utility in patients undergoing speech therapy or recovering from neurological insults.
The clinical versatility of lorazepam stems from its rapid onset and predictable kinetics. It is frequently used in the following therapeutic contexts:
Compared to other benzodiazepines, lorazepam has the advantage of not requiring metabolic activation by hepatic enzymes, making it suitable for patients with impaired liver function. Its clinical profile is marked by a clean pharmacokinetic curve, allowing for stable absorption, minimal accumulation, and consistent therapeutic effects. This is particularly relevant in neurorehabilitation, where fluctuations in sedation or motor control can interfere with task-specific exercises and patient participation.
Lorazepam is frequently integrated into speech-language pathology sessions, especially in cases where involuntary motor phenomena, severe anxiety, or hyperkinetic behavior disrupt structured tasks. By temporarily reducing these interferences, the drug enables greater focus, smoother articulatory patterns, and more efficient neuromotor coordination. It is not used as a standalone treatment for communication disorders, but rather as a pharmacological adjunct that allows rehabilitative efforts to proceed under more controlled neurophysiological conditions.
Lorazepam exerts its action by enhancing the effect of gamma-aminobutyric acid (GABA), the brain’s principal inhibitory neurotransmitter. It binds to the benzodiazepine site on the GABAA receptor complex, increasing the receptor’s affinity for GABA and thereby promoting chloride ion influx into neurons. This hyperpolarization decreases neuronal firing rates, resulting in anxiolytic, anticonvulsant, sedative, and muscle-relaxant effects. The modulation of central excitability occurs quickly after administration, which makes lorazepam highly suitable for acute symptom management.
The pharmacokinetic characteristics of lorazepam are particularly advantageous in time-sensitive clinical settings:
This metabolic profile contributes to lorazepam’s clean and predictable action, reducing the risk of drug accumulation in elderly patients or those with hepatic impairment. Unlike diazepam, which forms active metabolites that may prolong sedation or alter therapeutic timing, lorazepam maintains a consistent pharmacological effect that can be matched with therapy schedules. This predictability is crucial in neurologic and speech-language recovery programs, where timing of peak therapeutic effect often determines session effectiveness.
From a pharmacodynamic standpoint, lorazepam has a relatively high affinity for central GABA receptors, allowing it to exert strong clinical effects at low doses. Its sedative action is balanced by its ability to reduce motor overactivity and sensory hypersensitivity, conditions that frequently interfere with effective communication and rehabilitation. The result is a net decrease in neurologically driven interference, supporting clearer speech production, more controlled phonation, and less resistance to motor instruction.
Lorazepam is also used in treating neurological impairments that manifest with laryngeal tension, vocal tremor, or spastic dysarthria. By dampening hyperactivity in brainstem and extrapyramidal pathways, it improves the baseline neuromuscular state, allowing patients to produce speech with less strain and more control. When administered strategically before sessions, it creates a therapeutic window during which patients are most responsive to exercises focused on breath control, resonance, or articulatory sequencing. This targeted facilitation is especially beneficial in patients with post-stroke aphasia, traumatic brain injury, or progressive motor disorders involving vocal mechanisms.
For individuals managing chronic or episodic neurological conditions, consistent access to lorazepam can be critical in maintaining therapeutic stability. While traditionally dispensed through in-person consultations, evolving patient needs and logistical constraints have driven demand for secure and streamlined methods of acquiring the medication without interruptions. Whether used for seizure prophylaxis, acute anxiety, or to support structured therapy, lorazepam requires reliable delivery systems that align with both clinical requirements and patient routines.
With growing interest in convenient access to prescription medications, many patients consider ordering lorazepam online. However, because this drug belongs to a class of substances with a known potential for dependence and misuse, verifying the safety and reliability of online sources becomes especially important.
Patients seeking to buy lorazepam online must prioritize platforms that guarantee product authenticity, require valid prescriptions, and offer clear delivery protocols. Reputable online pharmacies typically operate under formal accreditation, source medications from licensed manufacturers or wholesalers, and provide documentation including batch number, expiration date, and manufacturer details. These platforms clearly list the available formulations (such as 0.5 mg, 1 mg, and 2 mg tablets), package sizes, and dosing instructions based on standard medical guidance.
One of the main advantages of using a verified online source is the availability of professional consultation prior to the transaction. While some websites collaborate with independent physicians who perform online assessments or video consultations, others accept scanned prescriptions issued by the patient's treating clinician. In either case, a responsible pharmacy will not dispatch lorazepam without evidence of a legitimate medical need. Absence of this requirement is a sign of a non-compliant and potentially unsafe vendor.
Another key aspect is delivery logistics. Established platforms provide customers with tracking numbers, delivery estimates, and customer support for shipment-related inquiries. Packaging is typically neutral and tamper-proof to ensure confidentiality and safety during transit. In most cases, delivery within urban areas takes 3–7 business days, while remote regions may require up to 10 days. Many services also offer express or overnight shipping options at additional cost. Reliable pharmacies maintain clear return and reshipment policies in the event of a failed delivery or damaged product.
Equally important is the transparency of the medication’s origin. High-quality suppliers make the manufacturer’s name, origin country, and registration number visible before purchase. This allows patients to confirm they are receiving an approved product rather than a generic or substitute without proper documentation. While generic lorazepam is medically equivalent to branded Ativan, buyers should be able to distinguish between them through labeling, appearance, and documentation. Color, shape, imprint code, and tablet scoring should match official pharmaceutical databases.
Finally, trustworthy vendors never attempt to upsell related medications or offer misleading “bundled therapies” without clinical justification. While lorazepam may be co-prescribed with antidepressants or mood stabilizers in psychiatric care, any such combination must be initiated by a qualified prescriber based on a thorough risk-benefit evaluation. Responsible pharmacies refrain from marketing language that implies enhanced effects through unverified combinations or misuse of the product’s anxiolytic properties.
Purchasing lorazepam online can be safe, effective, and discreet when done through a verified provider adhering to medical and logistical standards. Patients must remain vigilant for signs of illegitimacy, such as offers without prescription, unrealistic pricing, or lack of contact information. Consulting one’s primary prescriber before making an online purchase is strongly advised to ensure continuity of care and minimize health risks associated with unsupervised benzodiazepine use.
Ongoing access is particularly important in cases involving:
In each of these cases, patients and clinicians rely on continuity of medication to prevent regression, functional interference, or deterioration in therapeutic progress. Interruptions can lead not only to symptom reactivation but also to complications in coordinating care across disciplines.
When considering online acquisition, the selection of a reputable source is paramount. Indicators of a trustworthy provider include:
Patients seeking lorazepam online must avoid sources that promise unrealistic delivery speed, offer no medical oversight, or use vague terminology around product handling. Safe providers maintain clinical consistency by aligning with best practices in pharmaceutical distribution, even when accessed outside of traditional settings.
For those who use lorazepam strategically—such as before therapy sessions or during periods of increased neurological instability—timing of access becomes therapeutically relevant. A delay of even 24–48 hours may result in session cancellations or reduced therapeutic efficacy. Coordinating delivery with session planning ensures that medication is taken during optimal therapeutic windows, particularly when used to minimize speech-impairing motor events or anxiety spikes.
Some patients adjust their schedule based on known pharmacokinetics, for instance, taking lorazepam 45 minutes before articulation work or dysphagia therapy. In such use cases, dependable supply is not merely a matter of convenience but of preserving neurofunctional training momentum. Having predictable access empowers patients to remain engaged in therapy and responsive to cueing, physical tasks, or cognitive-linguistic goals.
Patients undergoing structured care for neurologically mediated communication disorders often require coordinated planning between physicians, therapists, and support staff. Integrating online lorazepam access into this workflow involves aligning refill schedules with therapy calendars, documenting treatment responses related to timing, and adjusting use based on clinical progress. In cases where lorazepam use is transitional—such as during early-phase aphasia therapy—online access supports gradual dose tapering aligned with functional gains.
Multidisciplinary programs benefit from predictability, and any logistical gap in pharmacological support can create unnecessary setbacks. Therapists may note decreased attention, increased dysfluency, or re-emergent anxiety symptoms when access is disrupted. Thus, for patients using lorazepam within a defined rehabilitative scope, reliable acquisition channels are not supplementary but foundational to success.
Lorazepam is a mainstay in the pharmacological management of several acute neurological presentations. Its rapid onset, high efficacy in modulating neuronal hyperexcitability, and favorable metabolic profile make it particularly suited for conditions requiring immediate intervention. Among its core indications are seizure disorders, panic reactions, and neurogenic spasticity that impairs functional communication and deglutition. These applications highlight the drug’s therapeutic breadth and its relevance in both inpatient and outpatient neurological care settings.
In seizure control, lorazepam is especially valued in the emergency treatment of status epilepticus and in secondary prevention among patients with unstable seizure thresholds. Administered intravenously or orally depending on urgency, it reliably suppresses ongoing epileptiform activity by enhancing GABA-mediated inhibition. Unlike phenytoin or valproate, lorazepam acts within minutes and does not require prolonged loading periods, which is crucial in time-sensitive environments such as stroke units, trauma centers, or intensive care wards. For patients with post-traumatic epilepsy, metabolic encephalopathy, or structural cortical irritability, lorazepam provides essential symptomatic coverage while other long-term agents are introduced.
In outpatient neurology and rehabilitation, lorazepam serves as a flexible adjunct for individuals with episodic seizure-related anxiety, subclinical focal activity with behavioral disturbance, or post-ictal disorganization. Its utility extends to supporting patients who exhibit prodromal neurological symptoms—such as focal twitching, vocal arrest, or motor instability—allowing early mitigation and preventing full seizure progression. In these contexts, lorazepam does not function as a first-line antiepileptic, but as a stabilizing support for therapy adherence and cognitive function preservation between episodes.
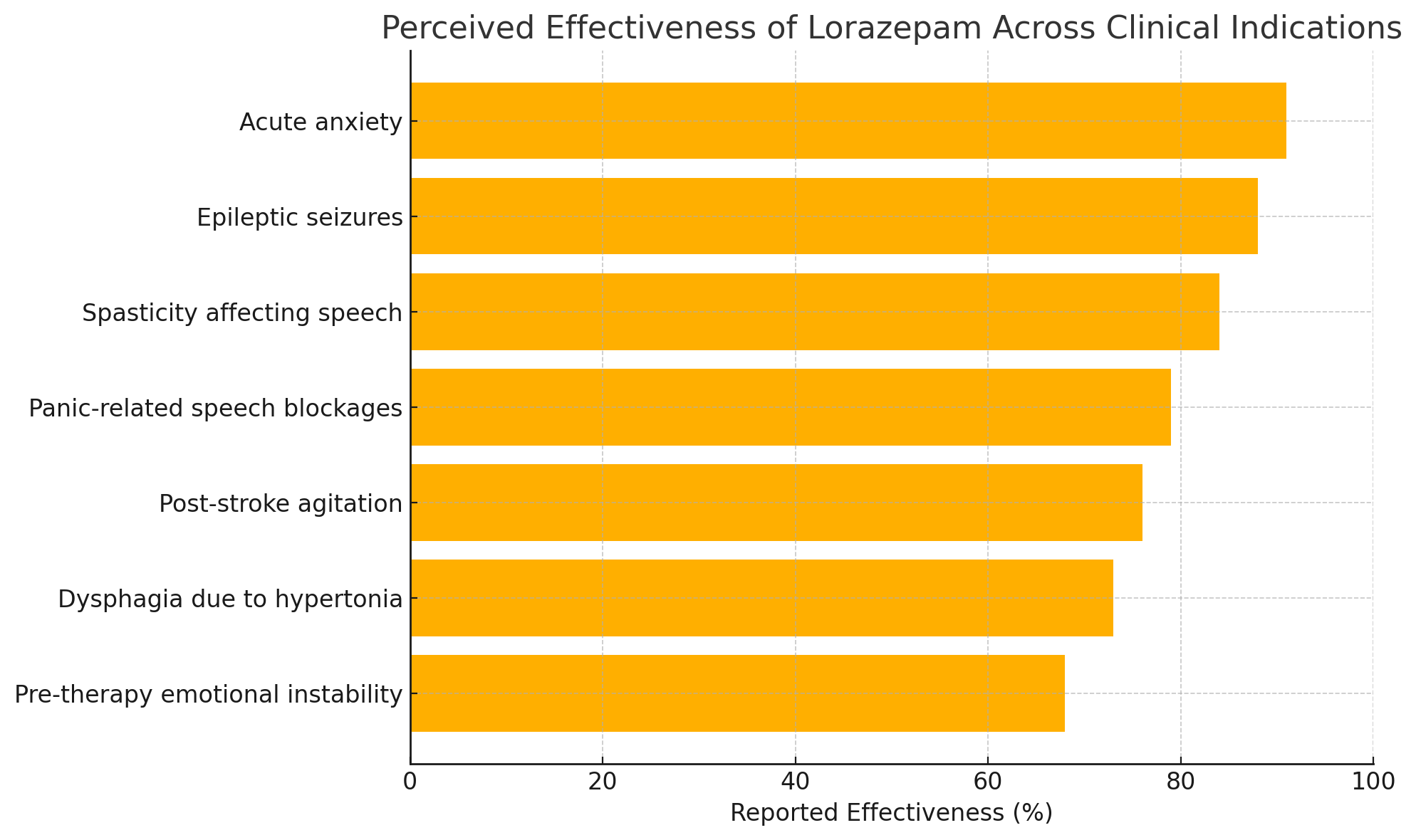
Its clinical use spans several key indications, where effectiveness is often reported by patients and clinicians alike. The following table summarizes perceived outcomes across major therapeutic applications:
| Indication | Reported Effectiveness |
|---|---|
| Acute anxiety | 91% |
| Epileptic seizures | 88% |
| Spasticity affecting speech | 84% |
| Panic-related speech blockages | 79% |
| Post-stroke agitation | 76% |
| Dysphagia due to hypertonia | 73% |
| Pre-therapy emotional instability | 68% |
The following chart visualizes the reported effectiveness across clinical indications:
Acute anxiety remains another key domain for lorazepam application. Unlike chronic anxiety syndromes managed with SSRIs or behavioral therapy, lorazepam addresses rapidly escalating autonomic dysregulation—tachycardia, hyperventilation, muscle rigidity, and perceptual narrowing—that compromises functional performance. In patients undergoing speech rehabilitation, this can manifest as vocal tension, articulatory freeze, avoidance behaviors, or physical distress during tasks. Short-term administration before high-demand sessions can prevent such manifestations, allowing patients to focus on instruction and task execution without overwhelming internal resistance.
In the context of generalized anxiety with somatic symptoms—such as gastrointestinal upset, chest tightness, or tremor—lorazepam supports the nervous system's recalibration during peak states. This is particularly useful in patients with speech-affecting anxiety syndromes such as selective mutism (in adults), conversion aphonia, or panic-induced disfluency. Here, the role of lorazepam is not to suppress speech behavior but to quiet the somatic substrate interfering with volitional control. Therapeutic gains rely on balancing anxiolysis with alertness, requiring precise titration and functional monitoring by the treatment team.
Lorazepam’s spasmolytic properties are leveraged in cases where oral or pharyngeal spasticity interferes with speech production or swallowing safety. In post-stroke bulbar syndromes, cerebral palsy with adult presentation, or upper motor neuron lesions, increased tone can impede phonatory coordination and lead to aspiration risk. Low-dose lorazepam can reduce this muscle overactivity without producing general muscle weakness. When coordinated with speech-language pathologists and dysphagia specialists, dosing is tailored to precede intensive oral-motor training or mealtime practice. This facilitates clearer articulation, smoother bolus transit, and more confident task participation.
Its use in this domain must be cautious, as excessive sedation or reduced reflex responsiveness can worsen deglutition risk. However, when administered with close supervision and in small, targeted doses, lorazepam enables more consistent implementation of therapeutic strategies and improves patient tolerance of challenging exercises. For instance, individuals undergoing thermal-tactile stimulation, effortful swallow techniques, or expiratory muscle strength training may show better compliance and coordination when muscle tone is moderated pharmacologically.
In sum, lorazepam’s applications in seizures, anxiety, and spastic interference are not limited to symptom relief—they directly enhance the accessibility and effectiveness of rehabilitative interventions. By reducing disruptive neurophysiological inputs, the medication clears a path for therapeutic work to proceed with fewer barriers and greater precision.
The integration of lorazepam into speech-language pathology is based not on direct modulation of language circuits but on its capacity to reduce interference from anxiety, motor hyperactivity, and spastic tension that obstruct effective communication. In patients recovering from stroke, traumatic brain injury, or exacerbations of neurodegenerative disease, speech production may be compromised by multiple factors—neurogenic aphasia, dysarthria, apraxia of speech, or behavioral withdrawal. When such impairments are further compounded by anxiety or excessive muscle activity, lorazepam may be used selectively to create a window of neuromotor and emotional stability conducive to productive therapy.
One of the most frequent applications is in post-stroke aphasia, particularly in early rehabilitation phases when emotional reactivity, task aversion, or speech-related frustration prevent full participation. In patients exhibiting limbic disinhibition, vocal outbursts, or avoidance of verbal attempts due to repeated failure, low-dose lorazepam can serve as a behavioral stabilizer. It facilitates initiation of structured expressive tasks such as automatic speech, object naming, or repetition drills. Speech therapists often observe improved tolerance of error, reduced vocal tension, and more sustained engagement when lorazepam is administered strategically before sessions.
In motor speech disorders, particularly spastic dysarthria, lorazepam’s muscle-relaxant properties may complement traditional rehabilitative techniques. By attenuating excessive laryngeal or articulatory tone, it enables patients to access clearer phonatory output, sustain voicing for longer utterances, and transition between sounds with greater precision. When combined with respiratory coordination training or resonance-based techniques, the reduction in spastic interference often accelerates functional gains. It also enhances the patient’s ability to respond to biofeedback, shaping vocal quality, rhythm, and amplitude in more stable conditions.
Lorazepam can be especially useful in patients with vocal tics, echolalia, or perseverative speech patterns triggered by anxiety or internal agitation. These symptoms often appear in neurological or psychiatric comorbidities such as Tourette syndrome, obsessive-compulsive spectrum disorders, or post-traumatic states. Short-term use of lorazepam may suppress the urge to repeat or interrupt, giving therapists space to introduce alternative strategies such as pacing, contrastive stress, or semantic priming. While behavioral methods remain the foundation of treatment, pharmacological support can reduce interference that otherwise delays acquisition.
In patients experiencing psychogenic speech suppression—such as conversion aphonia, speech arrest, or functional mutism—lorazepam may help unmask volitional capacity by reducing psychomotor inhibition. These cases require careful diagnostic differentiation, but in those where anxiety or hypervigilance plays a central role, brief pharmacological intervention can allow voluntary phonation to reemerge. This is particularly effective when paired with simultaneous behavioral activation, such as nonspeech vocalization, singing, or guided exhalation tasks.
Some patients in inpatient neurorehabilitation present with complex, mixed impairments—such as coexisting aphasia, apraxia, and hypertonic facial musculature. In such cases, lorazepam is not used uniformly but targeted toward the symptom cluster causing the greatest disruption to therapy. For example, in a patient with preserved linguistic function but severe oromandibular tension, lorazepam may unlock oral motor movement, allowing expressive function to emerge. In contrast, a patient with aphasia-related frustration but no motor component may benefit more from anxiolysis than spasmolysis.
Importantly, lorazepam is not used in isolation, nor is it administered daily without purpose. It is most effective when reserved for high-impact sessions, initial breakthrough phases, or in response to specific symptomatic surges. Therapists and medical staff collaborate to define the timing, dose, and duration of use, with functional outcomes such as speech intelligibility, therapy duration tolerance, and communicative intent serving as benchmarks of efficacy.
By reducing neurologically mediated barriers—both emotional and physical—lorazepam contributes to more consistent and focused rehabilitation. It facilitates the patient’s access to their residual communicative abilities and enables therapists to work more effectively within those limits. When timed appropriately and embedded within a goal-directed framework, lorazepam does not merely relieve symptoms—it helps restore the conditions in which speech and language can be rebuilt.
Lorazepam has established utility in acute neurologic care and palliative settings, where patients often experience abrupt changes in neurobehavioral state, involuntary movements, or distress that impedes both clinical assessment and functional communication. Its pharmacodynamic properties—rapid anxiolysis, reliable sedation, and motor dampening—make it a critical tool in managing neurologic instability when other interventions are insufficient or contraindicated. In these high-dependency environments, the goal is not long-term modulation but immediate symptom containment and preservation of patient dignity, comfort, and communicative access.
In stroke units and acute neuro wards, lorazepam is frequently administered to patients in post-ictal states, following cortical or brainstem hemorrhage, or during status epilepticus management. Patients may present with intense agitation, vocal restlessness, or dysregulated breathing patterns that interfere with examination and care planning. Lorazepam, given intravenously or orally, can quickly reduce these behaviors, allowing safer positioning, communication attempts, and basic interaction with care staff. Its onset within 20–30 minutes ensures timely impact, while its relatively short half-life allows clinical re-evaluation within the same treatment cycle.
Beyond seizures, lorazepam is employed in managing acute neuropsychiatric symptoms associated with traumatic brain injury (TBI), such as agitation, panic bursts, or involuntary vocalizations. In such cases, patients may exhibit behavioral dyscontrol that interrupts therapy, disorients caregivers, or exposes the individual to self-injury. Lorazepam can reduce these episodes long enough for therapists to reinitiate structured routines, conduct brief speech or motor assessments, or implement early interventions. It is particularly useful when patients are in transitional phases—exiting sedation but not yet fully oriented—and are prone to overreact to minimal stimuli.
In patients with degenerative neurological diseases such as ALS, multiple system atrophy, or advanced Parkinsonian syndromes, lorazepam is often introduced for episodic control of dystonic reactions, vocal spasms, or panic attacks related to respiratory compromise. These events often coincide with breakdowns in voluntary control, heightened emotional reactivity, and compromised communicative efforts. A well-timed low-dose of lorazepam can temporarily restore composure, allowing meaningful exchange, reinitiation of AAC systems, or guided swallowing interventions.
Palliative neurorehabilitation represents another domain where lorazepam is deployed judiciously. Patients at the end stage of neurodegenerative conditions may experience complex symptom clusters: restlessness, terminal delirium, breath-related panic, and disrupted vocalization patterns. When verbal communication becomes limited, nonverbal expression and physiological cues gain importance. Excessive anxiety, dyskinesia, or vocal struggle can obstruct this final phase of relational engagement. Lorazepam can be used not to silence, but to soften and clarify these expressions, allowing for better symptom interpretation, family interaction, and therapeutic closure.
In palliative speech-language care, lorazepam may allow short sessions focused on maintaining basic oral comfort, facilitating emotional expression, or supporting residual vocal function. These sessions often do not aim for recovery but for preservation—of identity, personhood, and communicative presence. Therapists may time lorazepam administration to coincide with bedside visits involving legacy work, farewell interactions, or breathing support instruction. The drug thus becomes part of a compassionate toolkit for maintaining connection when other modalities fall short.
The key to its effective use in these settings lies in tight interdisciplinary coordination. Lorazepam is prescribed and monitored by neurologists or palliative physicians, while speech-language pathologists provide feedback on functional response, communicative performance, and sedation thresholds. Dosages are kept minimal, and routes of administration (oral, sublingual, IV) are selected based on the patient’s condition and care goals. Success is not measured by symptom elimination but by the patient’s ability to remain communicatively present, safe, and calm within their clinical context.
Ultimately, lorazepam serves a stabilizing role when neurological fluctuations threaten communication, safety, or care continuity. In acute and palliative scenarios, its careful deployment reflects not merely pharmacologic intent but a therapeutic philosophy grounded in responsiveness, humanity, and the preservation of agency.
While lorazepam delivers substantial therapeutic value in acute and transitional settings, its repeated or prolonged use raises clinically relevant concerns. Chief among these are sedation, the development of pharmacologic tolerance, and impairment in cognitive and psychomotor performance. In rehabilitation and speech-language therapy contexts—where learning, memory, and consistent engagement are essential—these side effects must be anticipated, monitored, and minimized through careful dosing and strategic use.
Sedation is the most immediate and predictable outcome of lorazepam administration. Even at low doses, some patients experience fatigue, slowed verbal response, or generalized flattening of affect. In therapy sessions, this may present as reduced verbal initiative, diminished responsiveness to cueing, or difficulty sustaining attention to task. These effects are particularly problematic in early-stage recovery from stroke or TBI, where every communicative attempt builds momentum for reorganization. Sedation in such cases can suppress not only symptoms but neuroplastic potential, ultimately delaying progress.
Another key concern is tolerance, which refers to the body's adaptation to the drug, resulting in reduced effectiveness over time. Tolerance to lorazepam’s anxiolytic and muscle-relaxant effects may develop within weeks of continuous use. Clinicians and therapists may observe that a patient who initially benefits from a small dose eventually shows diminished functional improvement during sessions, requiring dosage escalation. This adaptation not only complicates pharmacologic management but increases the risk of withdrawal phenomena if the medication is stopped abruptly.
Patients who require intermittent support—such as before particularly challenging therapy sessions or during brief phases of increased symptomatology—can often avoid tolerance by limiting lorazepam use to defined therapeutic windows. This intermittent strategy maintains the drug’s clinical effect while preserving the patient’s underlying responsiveness and reducing physiological adaptation. Structured timing also facilitates easier tapering should lorazepam no longer be needed, minimizing rebound symptoms such as agitation, tremor, or insomnia.
Cognitive impairment associated with long-term lorazepam use includes slowed processing speed, impaired working memory, attentional shifts, and executive dysfunction. These deficits may not be immediately noticeable in low-dose, short-term use, but can accumulate over time—particularly in older adults or those with preexisting neurological damage. Speech-language pathologists frequently identify subtle cognitive inefficiencies during tasks requiring sequencing, metalinguistic judgment, or verbal problem-solving. These deficits may erroneously be attributed to primary neurological insult when in fact they represent modifiable medication effects.
Clinical teams must carefully distinguish between baseline neurologic dysfunction and pharmacologically induced slowing. Cognitive testing, structured observation, and comparison of medicated versus unmedicated task performance can clarify the true source of difficulty. If lorazepam-related dulling is confirmed, dose reduction or substitution with non-sedating alternatives may be considered. Behavioral strategies such as increasing session pacing, using more concrete cueing, and simplifying task demands can also partially compensate for slowed cognitive output in patients for whom lorazepam remains temporarily necessary.
Beyond cognitive and behavioral risks, lorazepam also carries a known liability for dependency, particularly in individuals with affective disorders, trauma histories, or prior substance use. While the drug is rarely initiated with abusive intent, its anxiolytic effects may become psychologically reinforcing in patients seeking immediate relief from internal distress. In speech-language therapy, this may take the form of patients requesting the drug prior to any task requiring expressive performance, even in the absence of significant anxiety. Such patterns require firm interdisciplinary boundaries and clear communication about the role and duration of pharmacological support.
Best practices in lorazepam use include: fixed short-term protocols, clear documentation of therapeutic rationale, ongoing functional tracking, and coordinated review between medical and rehabilitative staff. When therapy success depends partly on the timing and effectiveness of lorazepam, teams must ensure that benefits are not offset by cumulative risks. In all cases, the medication should serve the therapeutic process—not substitute for it.
Within the framework of multidisciplinary neurological care, lorazepam serves not as a primary therapeutic intervention, but as a strategically positioned adjunct that facilitates access to core rehabilitative modalities. Its greatest value lies in time-limited, targeted application—where reducing neurological overactivation enables patients to more effectively engage with therapy, comply with structured tasks, and tolerate symptom-specific interventions. When used judiciously and with functional endpoints in mind, lorazepam enhances clinical outcomes by removing physiological and behavioral obstacles that impede recovery.
In speech-language pathology, occupational therapy, and neuropsychological rehabilitation, patients often struggle to benefit from evidence-based interventions due to involuntary movement, severe anxiety, or cognitive agitation. These states create barriers to compliance, distort task execution, and prevent the establishment of new neural pathways. Lorazepam acts as a chemical buffer, temporarily suppressing these interferences so that therapists can implement motor retraining, speech drills, or cognitive-linguistic strategies in a more stable context.
The medication’s clinical success depends heavily on timing. Its relatively short half-life allows practitioners to administer lorazepam 30 to 60 minutes prior to sessions where active participation is crucial. Examples include:
What differentiates lorazepam from passive pharmacologic agents is its ability to support active skill-building during its therapeutic window. Unlike long-acting benzodiazepines, which may blunt responsiveness throughout the day, lorazepam can be confined to specific timeframes where its benefits are maximized and side effects minimized. This allows therapists to structure sessions around pharmacodynamic peaks, increasing the likelihood that neural changes will occur under optimal conditions.
Rehabilitation protocols that include lorazepam do so with defined goals: reduce dyskinesia during motor retraining, improve phonatory consistency, or stabilize affect during verbal output. Once those goals are met—or once patients demonstrate sufficient adaptation—use of lorazepam can be tapered or discontinued entirely. This built-in reversibility is a clinical strength, supporting functional independence without long-term pharmacologic dependence.
Successful implementation requires team coordination. Prescribing clinicians must communicate closely with therapy staff to align timing, monitor side effects, and assess when benefits plateau. Therapists, in turn, report on performance variables that reflect pharmacologic impact: session duration, task accuracy, initiation latency, and tolerance of novel demands. These data allow for real-time decisions about dose modification, session scheduling, and treatment trajectory.
Patients themselves are educated on the purpose of lorazepam within the therapeutic plan. They are informed that the medication is not a long-term solution, but a short-term enhancer of therapeutic access. This framing helps set expectations, reduces requests for continued use beyond necessity, and reinforces the importance of active participation in the rehabilitative process.
When integrated properly, lorazepam enables breakthroughs that would otherwise be postponed or rendered unreachable due to overwhelming internal interference. It creates an entry point—a narrow but powerful interval—during which therapists can recalibrate movement, rebuild expressive function, or shape cognitive response. Its role is not to mask dysfunction, but to stabilize the environment in which recovery can occur. Within the hands of a skilled interdisciplinary team, lorazepam serves not as a crutch, but as a calibrated clinical tool—supporting the patient only long enough to regain their own forward momentum.